Not sure if disease outbreaks can radically change our attitudes about the physical design of buildings and interior environments?
It can. Just ask architecture and interior design historians.
Many of the design innovations we take for granted (from non-porous linoleum flooring to seamless ceramic sinks) found in today’s modern laboratories, kitchens, and bathrooms first became standard design features as a result of major disease outbreaks in the early 20th century, including tuberculosis and Spanish Flu.
These rapid changes were based on the best scientific research available at the time.
While the exact nature of viruses had yet to be determined, there was a new appreciation (and fear) of the havoc caused by bacteria, which, in turn, drove a new “clean” revolution in interior design and sanitation, created to rid interior spaces of dangerous disease-spreading germs.
Victorian-era interiors, with their preponderance of dark rooms, laden with curio collections, intricately carved wood furniture, heavy carpets, and drapery were suddenly out. They were replaced with gleaming white hard surfaces that were easy to clean and sterilize — including white subway tile on the walls, ceramic honeycomb tile or hard linoleum on the floors, porcelain plumbing fixtures (molded without exposed seams where germs could lurk), stark white painted walls and ceilings – all of which remain in use to this day.

Bright overhead electric lights made dirty surfaces easy to spot, as did the new bleached white coats and white uniforms worn by doctors, lab workers, and nurses (which replaced the black coats and dresses worn by their predecessors during the Victorian era).
This clean, modern design philosophy, which first took hold in hospitals, laboratories, and sanatoriums, began to influence the design of 1920s offices, bathrooms, and kitchens, e.g. areas that were particularly suspect when it came to disease transmission.
Indeed, many architecture and design historians point to this era of “sanitation design” as the foundation of what would later become the modernist design movement in architecture, led by the Bauhaus school and beyond.

So, if people tell you a disease outbreak won’t change how we design our buildings and interiors, they’re wrong. It’s happened before and can happen again.
So how will Covid-19 affect laboratory as well as other clinical and pharma facility designs?
Although Coronavirus can spread by contacting virus-laden surfaces (e.g. fomite transfer), the primary means of disease acquisition appears to be via the respiratory system: coughing, sneezing, singing, and even loud talking can hasten the spread of the virus from one person to another. Worryingly, new research also shows that flushing an open toilet can also create a cloud of potentially infectious aerosol droplets.
3D simulation illustrates how microscopic aerosol droplets (potentially carrying the Coronavirus) float in the air as people in close proximity sneeze, cough, or converse with one another.
Given enough time, the droplets containing virus particles will dissipate, either dropping to the floor or getting swept up into the ventilation system. Any virus particles landing on a working surface can be cleaned with sanitizing agents (with quaternary agents being especially effective) or they will simple “die” on their own in a matter of hours or a few days.
Why do we mention these details? The reason is that in the laboratory context, once a risk is understood, it’s a straightforward process to plan and carry out measures to limit the risk due to dangerous conditions (e.g. keep lab workers safe), or to prevent cross-contamination (e.g keep experiments accurate and reproducible), etc. etc.
This kind of risk mitigation happens every day in laboratories around the world. After all, bio-safety labs deal with much more dangerous pathogens; chemists handle noxious materials with potentially fatal fumes, and blood labs implement procedures to protect workers from exposure to hepatitis and HIV viruses.
Working with Coronavirus is no different. Once the “rules of the road” are established, labs can make the necessary changes to reduce the risk of the virus transferring from person to person.
So how will these changes take place?
We take a look at eight different components to consider when preparing your lab to deal with the risk of the Covid-19 virus, from layout changes to behavioral changes, to new safety and work scheduling procedures.
1. Revise Physical Layouts to Control the Spread of Coronavirus in the Laboratory
New safe operating guidelines from the CDC and OSHA recommend specific changes to the interior design layouts of businesses (including laboratories).
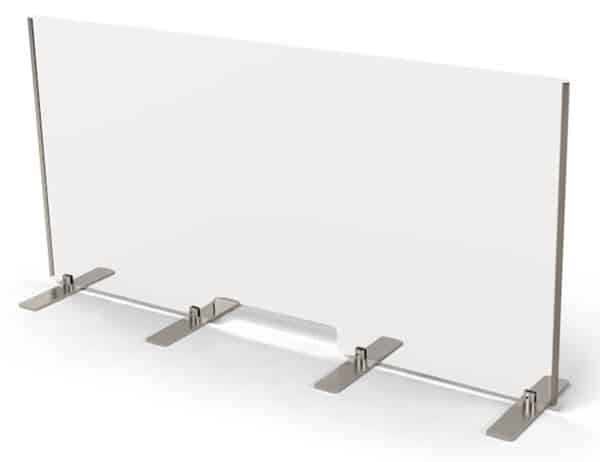
These include new practices for implementing social distancing in the workplace, such as spacing workers 6 feet or further apart, or providing transparent divider shields when that’s not possible.
(Laboratory managers will also want to take note of special CDC recommendations for laboratories handling Covid-19 specimens, such as testing labs.)
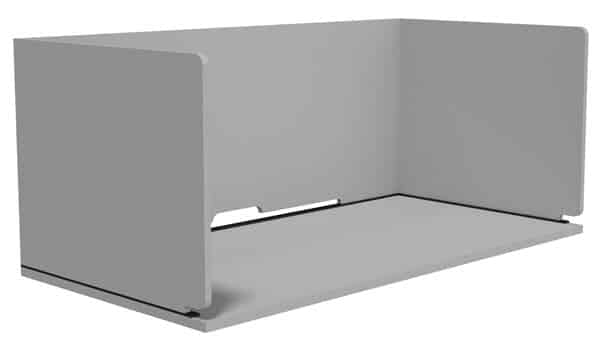
For years, Formaspace has been spreading the gospel of modular furniture design for laboratories. Why? When you need change, modular designs are very easy to reconfigure. And, given the reality of the current pandemic, that time has unfortunately come.

In response to the pandemic, we’ve created new product features for our lines of modular lab workbenches – such as transparent shields — which can also be easily retrofitted to any existing installation in the field. (Speak to your Formaspace Design Consultant for specific recommendations.)

If you have different types of laboratory furniture installation, such as custom casework furniture or furniture lines from a different manufacturer, we also offer a series of retrofit products that can provide additional protection for your lab workers.
Facility managers are also making other changes to physical layouts; for example, where there is space, many are installing airport-style doorless restroom entrance and exits as well as electronic faucets, to increase ventilation and eliminate the need to touch door handles or faucets.

While certain categories of laboratories, such as cleanrooms or bio-safety labs, already have gowning rooms, facility managers are looking at adding dedicated areas for lab workers to put on or take off their PPE (e.g. donning and doffing areas).
2. Create More Personal Space for each Individual Worker
Ten years from now, we may look back at this period and say this was the beginning of the end of “open plan” laboratory designs.
Open plan lab designs have become popular for a reason, actually, several reasons. They encourage “Team Science”-based collaboration, make better use of limited resources (by allowing more efficient sharing of increasingly expensive test equipment, for example), and can help labs operating in high-cost bio-tech clusters (such as Boston, for example) constrain their expenditures on expensive real estate by fitting more personnel into the same square footage.
But the Coronavirus pandemic makes many of these arguments seem uncomfortable, or out of date.
To maintain proper social distancing and to prevent viral transmission at work, lab workers actually need more personal space. They are also less likely to want to share equipment, and they have an increased need for secure personal storage — for their own PPE, for lab notebooks, or for anything else that they would be handling.
One easy change to make is to reduce the number of lab workers seated at a single workstation; if you currently have two technicians sharing a workstation, you could reduce that to one (to maintain social distancing).
But how can you accommodate the displaced worker?
There are options.

Mobile workstations with industrial-strength castors can be part of the solution. These can also be equipped with built-in storage areas to keep PPE and other personal items secure.

Formaspace also offers a line of modular lab systems, such as our Triton line, which makes it easy to add an additional sink in a wet lab environment.

Our FabWall system is another option; it creates a strong, modular backbone structure to which you can add workstation elements, including monitor stands, shelves, and storage components.
Take a moment to speak to your Formaspace Design Consultant for more detailed recommendations.
3. Empower Team Leadership and Encourage a Problem Solving Mindset
Changes brought about by the Coronavirus pandemic are not insignificant, but they are not insurmountable either.
Many laboratories already mitigate significant risks associated with their core missions. For example, laboratories performing animal studies must ensure that their vivariums are secure to prevent animal to human transmission of diseases or other cross-contamination that could render experiment results invalid. Personnel working in bio-safety labs or clean rooms know how to follow detailed standard operating procedures (SOPs) to prevent accidental exposure to pathogens or unintended contamination of sensitive experiments. And the list goes on, from labs handling blood products (as we mentioned earlier) to labs working with radioactive materials, explosive chemicals, and so on.
Our point is that laboratory professionals know how to take precautions.
Establishing a task force that’s empowered to develop appropriate Standard Operating Procedures to address Covid-19 specific concerns is the first place to start. Bring together experts from different disciplines, such as Environment, Safety, and Health (ES&H) professionals, to ensure a wide range of viewpoints are carefully considered.
As operational guidelines are developed, it’s important to test any new SOPs against any potential infection scenarios by performing a root cause analysis.
Challenging thought exercises such as these will help to ensure safety in your laboratory. Remember, while most traditional risks to health and safety in the laboratory are associated with external sources (such as pathogens in a test tube or dangerous chemical fumes), each of us has the potential to be a source of infection when it comes to Covid-19.
What happens if an asymptomatic lab worker comes to work without any apparent symptoms, e.g. no temperature and no loss of taste nor smell? What would be the consequences of this happening with respect to your plans? For example, have you considered the steps necessary to track and trace who this person came in contact with in the laboratory once the infection is discovered?
Tip: consider strategies used successfully in other industries as well. For example, in many hospital systems and throughout the airline industry, there is a “no-fault” policy that allows professionals to come forward (without retribution) when they make a mistake in an effort to increase the body of “lessons learned” knowledge and to help prevent a future occurrence.
Another system that originated in the automotive industry might be useful for reducing contamination in laboratories: the 5S program, a step-by-step procedure to make any workplace more efficient. The use of the 5S approach in a laboratory might help you uncover ways to optimize materials and equipment storage; this analysis might show, for example, that placing small supplies of common chemical reagents at each workbench in a wet lab could cut down on the number of trips needed to replenish supplies at a central location, thus helping improve social distancing throughout the lab.
4. Limit Covid-19 Exposure Hours
This brings us to another important point about improving worker safety during the Covid 19 pandemic.
The risk of transmission between two individuals increases with the amount of time they’re exposed to one another. You can think of this as “Covid-19 exposure hours.”
The more Covid-19 exposure hours you accrue, the greater the risk you face in acquiring the virus.
You can think of it this way, a quick trip to the store is likely to be less risky than a long visit to a restaurant where you interact with the serving staff and other patrons.
This is why many lab managers, like their counterparts in other business sectors, are implementing work from home (WFH) policies and limited or staggered shifts for on-site workers.
In other words, having fewer workers on-site automatically limits the overall number of Covid-19 exposure hours at your facility, reducing your net risk level.
But how practical is working from home in a laboratory?
The answer is it depends. Many laboratory job functions, such as data analysis, research and planning, grant writing, or communicating with other scientists at different laboratories, can be performed outside the lab.
But that does leave quite a few tasks that have to be done in the lab, whether it’s managing automated testing equipment or performing intricate experiments. The question becomes “how many people have to be in the lab at the same time?”
Lab managers labs have to ask themselves some hard questions.
For example, is it still a safe practice to rely on relatively large numbers of graduate students (working off their stipends) to perform run-of-the-mill lab duties (which creates a crowded environment)? Or should financial resources be allocated toward employing one well-trained, highly versatile lab technician who could perform these tasks alone?
5. Stop the Virus at the Source
As we mentioned earlier, many laboratories use some form of personal protection equipment (PPE), whether it’s a hazmat suit in a biosafety lab, a fume hood in a chemistry lab, or gloves in a clinical testing lab environment.
Depending on your circumstances, you may need to provide (as mentioned above) a PPE donning and doffing area so that your employees can put on their protective equipment prior to entering the lab work environment.
Video demonstrating the proper procedures for donning and doffing PPE in a clinical testing environment. Your laboratory facility may be using equipment such as this already, or it may be a new policy require their use on the job
Two of the most effective ways to prevent Covid-19 virus transmission also happen to be the simplest and cheapest measures you can take:
First, wash your hands for 20 seconds or more several times each day — and definitely before you eat or drink anything (it’s also important to learn how to avoid touching your face in between washing sessions). If it’s possible, you should invest in kitting out your laboratory with additional sinks to encourage handwashing; the next best choice is supplying sanitizing gel at convenient locations throughout your laboratory.
The second most important way to stop the virus spread is by wearing masks while at work.
It’s important to emphasize to lab workers who are not familiar with the mechanics of face masks that wearing a mask protects others from your germs, not the other way around. In other words, when you sneeze or cough, the mask that you wear helps prevent those germs from spreading into the air. Most masks, however (aside from the highly sought-after surgical N-95 masks), do not prevent you from breathing in the virus.
6. Step Up Hygiene Protocols
Keeping a laboratory neat and tidy comes as second nature to most laboratory scientists and technicians. Why? Maintaining a clean environment is crucial in preventing cross-contamination, which can ruin experiments and data collection efforts.

Most laboratories can extend their existing sanitary hygiene programs to incorporate steps to prevent fomite transmission of Covid-19 virus fairly easily.
Greater emphasis will have to be placed on cleaning high touch areas, such as our personal phones, keyboards, mice, and so on. Items that are commonly touched (so-called high touch surfaces), such as refrigerator handles, restroom door handles, water faucets, or elevator control panels, all need to be cleaned multiple times a day using EPA approved cleaning materials, such as quaternary disinfection treatments.
As mentioned earlier, there’s new research that toilets can admit a cloud of aerosol when flushed with the lid open. Since many toilets used in commercial spaces have a ring but no cover, it may be advisable to install covers and instruct all employees to close the lid before flushing.
Other changes in the restroom include the use of touchless faucets, touchless soap dispensers, removal of forced air hand dryers (which can blow the virus around) in favor of automatic paper towel dispensers, as well as increased ventilation throughout the restroom.
Laboratories that are not using UV light-based disinfection systems, now common in hospital settings, may want to investigate their use. These systems, which we wrote about in a recent article, allow rapid disinfection of a broad area in as little as five minutes.

You can also take a look at the furniture used in other areas of the laboratory as well. Are the worksurfaces easy to clean and sterilize? Are the floors made of materials that can be sanitized effectively? What about seating systems, are they upholstered with difficult to sterilize fabric? Furniture upholstered with porous materials, such as leather or fabric, are problematic when it comes to sanitizing.

Instead, we recommend our line of Formaspace seating products, which are specifically designed for laboratory and cleanroom use thanks to their unique soft molded plastic surfaces that are comfortable to sit on yet can easily be sanitized using normal cleaning products.
7. Improve Air Flow and Filtration to Reduce Viral Transmission
When it comes to controlling virus particles in the air, cleanroom laboratories are already a step ahead in the game: cleanrooms have the high airflow necessary to rapidly “pull” virus particles down to the plenum underneath the floor, where they are either expelled to the atmosphere or filtered through high-quality HEPA filters before being recirculated back inside the facility.
Other laboratory facilities would do well to emulate the cleanroom approach. There’s some evidence that downward directed air movement is superior when it comes reducing viral transmission. This airflow directs virus particles to the floor and away from our mouths or nostrils.
Laboratories with energy-saving HVAC systems may want to reprogram their air control systems to maintain a “fast” airflow setting; this won’t be as energy efficient, but it will keep airflow moving, which is thought to help prevent high concentrations of aerosol droplets that could lead to viral transmission between lab workers.

Finally, installing HEPA filters to treat the conditioned air returning through the HVAC system can help eliminate recycling the virus back into the laboratory environment.
8. Invest in Virtualization and Automation
Automation and virtualization have become a fact of life in much of our day-to-day laboratory work, but there are opportunities for lab facilities to take these advances further.
For example, many laboratory test equipment manufacturers offer remote access options, so that researchers and lab technicians can monitor the equipment from outside the laboratory (such as when working from home). We predict this trend will accelerate as laboratories retrofit existing equipment or make purchasing decisions based on these features.
We’re also seeing a move toward virtualized meetings. Whereas it was quite common in the past for researchers to gather in a conference room to communicate by teleconference with their colleagues at another institution, the trend now is for individuals to participate in Zoom meetings. This trend is firmly established now during the lockdown period and is expected to grow even more important.
Automated employee management systems will also become more important.
It’s becoming more common to leverage worker access badges or smartphone software to track employee whereabouts. Newer systems also incorporate new optional features, such as instructing workers where to sit for a particular work shift. And vendors are busy adding new features that are virus-specific, for example, keeping track of which employees you may have come in contact with during work hours, which could provide vital information to track and trace a potential viral exposure.
Finally, the pandemic will most certainly accelerate the trend toward developing so-called smart laboratories that feature greater end-to-end automation. (TIP: You can read our reports on laboratories of the future here, and creating smart laboratories here.)
Turn to Formaspace for Help
When you need to make changes to your lab quickly, Formaspace is ready to respond rapidly.
For example, when General Motors asked us to build 500 workstations for their new ventilator facility in Kokomo, Indiana, we delivered the project in just 18 days.
Our factory headquarters in Austin, Texas is ready to assist you with your project needs, whether you want to update an existing laboratory or create an all-new facility from scratch.
Find out why prominent laboratory customers, from Medtronic to Roche, choose Formaspace for their laboratory furniture needs.
Contact your Formaspace Design Consultant today.