As the 30th annual Healthcare Facilities Symposium & Expo gets underway here in Austin, Texas, we take a look at the intersection of technology and healthcare to ask some tough questions: Are digital health solutions reaching their full potential? Is virtual reality in healthcare just hype? Will the Internet of Things (IoT) advance the delivery of quality care?

In an era when the Internet is upending industries, from hotel accommodations to grocery sales and transportation services, many healthcare industry analysts and entrepreneurs have been championing a similar revolution in digital healthcare.
Let’s take a survey of the progress that’s been made in advancing technology and healthcare since the enactment of the Affordable Care Act (ACA) in 2010.
Are More Streamlined IT Apps for Healthcare Providers and Payers Coming?
Whether you are a supporter or detractor of the ACA legislation, some of its lesser-known provisions (lesser-known outside the healthcare world that is) have tried to steer the big ship of healthcare away from the traditional “fee for service” model by offering healthcare providers new financial incentives (such as those offered by Accountable Care Organizations, known as ACOs) to focus on the quality of patient outcomes. (There have also been major reimbursement penalties for obvious care lapses, such as re-admitting patients within a few days after a hospital discharge.)
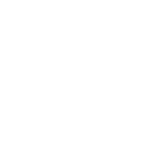
The ACA has also incented providers (by tweaking reimbursement rates) to adopt electronic healthcare record (EHR) systems — as long as they can provide a paper trail demonstrating what is known as “meaningful use.” This comes at a time when new coding standards for categorizing treatments, known as ICD-10, have been rolled out — much to the delight of “big data” evidence-based medical researchers but to the chagrin of care providers who have had to scramble to train personnel to learn the new coding procedures.
From a digital health perspective, these changes have been a golden opportunity for EHR software vendors (particularly for Minneapolis-based EPIC, the 800-pound gorilla of EHR systems), but those hoping that electronic healthcare records would be a springboard for consumer convenience and choice have generally been disappointed.
Despite widespread adoption of electronic healthcare records, the average consumer still finds it difficult to transfer their medical records to a new healthcare provider. While regional Healthcare Information Exchanges (HIEs) try to badger the healthcare systems to participate in record sharing, they’re often reluctant to let go of their captive markets. Interoperability is also a low priority for many EHR vendors as well (and from their perspective, why not?) — many of them use lowest-common-denominator methods, e.g. dumb data “screen scrapes,” to transmit records between their systems and those of their competitors.
Given all this complexity, it’s been difficult for entrepreneurs to enter the healthcare market and create apps that are the “UBER of healthcare.” And this is before talking about the Federal government’s stringent patient privacy regulations, collectively known as HIPAA (the Health Insurance Portability and Accountability Act of 1996). HIPAA has been a final nail in the coffin for many digital health entrepreneurs contemplating entering the healthcare market, as the penalties for data breaches are quite onerous. (Consequently, as we’ll see below, most consumer product companies, such as Apple and FitBit, have focused their efforts on fitness apps, which operate outside the reach of HIPAA regulations.)
Entrepreneurs and marketing-types who move into the healthcare realm are also surprised to learn how much sway the reimbursement rules from the Federal government’s CMS (Centers for Medicare & Medicaid Services) have over what can or cannot be offered to healthcare patients. You can’t offer free toasters for changing doctors in the CMS world – nor can you offer incentives for seemingly benign items either, such as tokens to pay for garage parking.
Low CMS reimbursements are also causing structural changes in the primary care segment. More and more physicians, frustrated by low reimbursement rates, are electing to convert their practices to what is known as “concierge care.” Concierge practices require patients to make hefty annual upfront cash payments — typically ranging from $1,000 to as much as $3,000 annually. Those who can’t afford it (which includes most Medicare/Medicaid patients or those with insurance plans) are left behind to find care elsewhere.
In light of all these complexities, is anyone even trying to bring an “UBER”-like digital health experience to healthcare delivery? One bright spot is Oscar, the healthcare insurance company that is trying to brand itself as a digital health community.
Physician Extender Technology and Healthcare Delivery Outsourcing and Automation
Given all these barriers to entry in the healthcare market, are there any other opportunities for digital health innovation?
The answer is yes.
Today, healthcare leaders are facing an industry that is undergoing significant change driven by: public/private pressures on cost, quality, access; focus on reducing costs by managing health; increasingly changing reimbursement models; and integrated health through collaboration with health plans and clinical delivery.
With primary care providers stretched thin by low reimbursement rates, most have ramped up the number of patients they see each day by using what is euphemistically known in the industry as “physician extenders.”
In many cases, physician extenders are real live human beings, with job titles such as Nurse Practitioners (NPs) and Physician Assistants (PAs) who can take patient histories, make diagnoses and, in the case of NPs, prescribe medications (under the doctor’s supervision).
A new job category has also emerged, the medical Scribe. Scribes, who are trained in medical terminology, shadow the physician, NP or PA to capture and enter patient information (and survey data mandated by the ACA) into the EHR systems.
In time, it’s likely that advances in artificial intelligence (AI) and natural language systems will assist or even replace the role of the human scribe. Other resource-intensive tasks that are mandated by ACA regs, such as providing diabetes counseling, could also be handed off to robotic counselors.
What about apps to extend the reach of the physician?
Telemedicine is a great example. Why should you even come into the office when you could Skype or Facetime the doctor instead?
It turns out the widespread adoption of telemedicine is held up by regulations to some extent. For example, patients must have an established relationship with a doctor before they can use telemedicine (e.g. they must have already had at least one in-person visit). Another requirement: Communication software and hardware vendors have to assume responsibility for maintaining HIPAA patient privacy — yet major software companies (Microsoft with Skype) and (Apple with Facetime) have declined to do so, despite the fact that their apps are sufficiently encrypted for the task. Without a clear industry leader, telemedicine adoption rates have been slow to take off.
Interestingly there have been more advances in first responder systems that connect a remote physician to EMT personnel at the scene of an incident.
Houston’s Project ETHAN leads the way for telemedicine solutions that allow emergency responders to focus their resources more efficiently.
What about AI systems interpreting x-rays or providing differential diagnoses for patient illnesses? We’ll talk about that in the “Big Data” section below.
Advances in Delivering on the Promise of Personalized Medicine and Genomics
Many analysts believe the future of healthcare lies in personalized medicine.
And why not?
Each of us has a slightly different genetic makeup.
Companies such as 23 and me have popularized home DNA testing (to learn about our ancestors, for example).
But DNA testing offers much more. It’s the basis of the emerging field of genomic medicine, which attempts to match each of our unique set of genes with a corresponding treatment protocol that will deliver the most beneficial outcome.
Leading oncology institutions, such as Houston’s MD Anderson Cancer Center in the Texas Medical Center, have been at the forefront of genomic research.
By testing patients for their genetic characteristics, MD Anderson has been able to create specific treatment regimens, particularly in breast cancer cases.

For example, as we’ve written about before, direct gene manipulation for human embryos is on the horizon, using CRISPR gene editing technology.
Our deeper understanding of diseases at the gene level is also helping to bring surprising cures, such as the recent development of a pill that can suppress Hepatitis C in many patients. (The eye-watering cost of these treatments is an important topic for another day.)
What else is on the digital health horizon?
Miniaturization and meta tests/vaccines are coming. For example, pill-sized cameras that can be swallowed are an emerging alternative to catheter-based cameras. And, despite the humiliating $9 billion setback of the once high-flying start-up, Theranos, blood tests that can identify a lifetime of exposure to viral and other infections are on their way, as well as meta vaccines, which can provide protection against a large number of illnesses with a single injection.
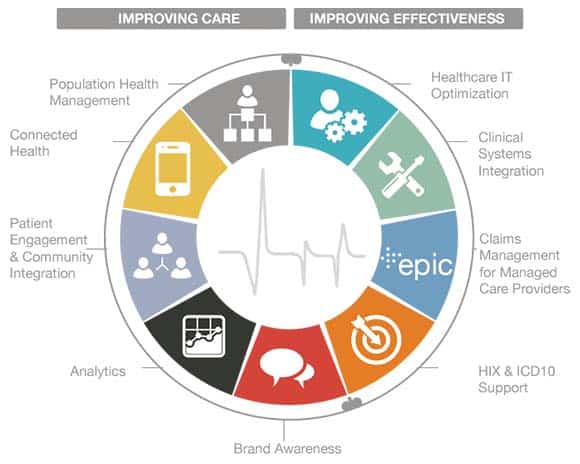
Widespread Adoption of IoT Connected Digital Health Devices
What about the hype associated with the Internet of Things (IoT)? Will connected devices take off as the next big thing in healthcare?
Regulations are dividing the marketplace into two camps.
On the one hand, we have the category of FDA approved medical devices; these require entrepreneurs to make a significant investment in patient testing for safety and efficacy. Make no mistake, these connected devices are cool. They can provide long-term monitoring of things like heart-conditions and transmit the data directly to the doctor for interpretation. The possibilities don’t stop there — check out the TMXc and JLabs healthcare innovation incubators for some of the latest new devices coming to market. (FYI we’ll talk about artificial organs, such as prosthetic eyes and ears, in a section below.)
But, for many Silicon Valley entrepreneurs, that’s a less attractive category than the health, fitness and wellness segment, which does not require FDA oversight. That’s why we see consumer product developers, such as Apple with their Apple Watch, FitBit with their myriad lines of fitness trackers, as well as health-oriented apps, such as MyFitnessPal and Lose It! make their financial investments in consumer-grade fitness devices and apps. For them, it’s lower hanging fruit, e.g. a bigger market that avoids the need for complex FDA compliance.
Of course, we are not advocating for reduced oversight of patient safety.
But it will be a while before some of the best and brightest (and most well-funded) minds of top Silicon Valley companies enter the FDA approved medical device marketplace.
What health devices are we missing out on while consumer electronics entrepreneurs scoop up all the money from the non-regulated market?
That’s something to think about when you take your dog to the veterinarian, and they insert a quick blood draw from your pet into a miniaturized, automated lab testing device – these devices can spit out a report on your pet’s blood levels as well as liver and kidney function in a few short minutes. Why don’t human healthcare consumers have access to that level of technology?
Use of Virtual Reality in Healthcare Delivery and Medical Education Settings
At a time when Baby Boomer physicians are retiring in greater numbers, healthcare industry analysts have been forecasting a looming shortage of primary care physicians to meet the needs of an expanding population.
Many see medical education as one of the primary uses for virtual reality in healthcare.
For example, Stanford has developed a virtual heart application that lets medical students walk around and interact with the complex features of the heart, its arteries, and veins, as well as simulations of common heart disease conditions.
Stanford’s David Axelrod, MD presents the Stanford Virtual Heart at the 2017 CeBIT international medical device conference held bi-annually in Germany.
Virtual reality (VR) can also help medical professionals visualize live patient data. New systems can combine results from MRI or CT scans and project them into a visual environment that allows care providers to closely investigate 3D images of their patients without having to perform invasive exploratory surgery. VR simulations can also help surgeons pre-plan operations by visualizing each step in advance of the procedure.
The addition of haptic (e.g. force) feedback tools and high-speed data connections are underlying technologies behind “telesurgery” — a system where a remote surgeon can perform an operation on live patients by viewing the patient on a camera while manipulating surgical cutters using haptic controls.
VR is poised to make inroads in other areas as well:
VR can assist in treating mental illness by providing flexible, low-cost exposure therapy that can help reduce anxiety and panic attacks, making it an ideal solution for patients suffering PTSD.
The same approach can also apply to pain management. VR can provide patients who experience debilitating pain symptoms, such as burn victims, with a drug-free “distraction” therapy. This often takes the form of interactive games, which are designed to distract the mind away from the pain symptoms. Similar techniques are being used to treat physical therapy patients.
The “Big Data” Approach to Evidence-Based Medicine
Long the dream of many medical researchers, an “evidence-based medicine” approach to healthcare is well positioned to become the norm — if we want it to — thanks to a confluence of increased data collection (think EHRs and ICD-10 coding standards) combined with advances in neural network powered “big data” computing power.
The idea on its face seems reasonable. Large anonymized patients’ data sets are reviewed to correlate discernible relationships between positive (or negative) medical outcomes that result from various medical treatment protocols. In other words, you try to identify which treatments give the best results and promote them over other approaches.
It’s not been without controversy. During the debate over the ACA, critics latched onto provisions that would pay care providers for something they weren’t previously getting paid for, e.g. providing end-of-life counseling on important topics like setting up medical directives (such as whether one is to be resuscitated or not.) Critics recast this as government interference in the doctor-patient relationship (which is true only to the extent that CMS was offering to pay a fee for a service, like every other type of fee for service payment they make) with some going so far as calling it a government “death panel.”
This false aspersion has hijacked what should have been a national conversation on the role of CMS departments, such as the National Committee on Vital and Health Statistics (NCVHS), and other committees which make important decisions on how our healthcare dollars should be applied for maximum benefit.
Despite this, there are promising developments in “big data” for digital health, some of which certain healthcare specialists may come to regret.
Increasingly, computers powered by artificial intelligence algorithms can meet or exceed the capability of human radiologists in interpreting x-ray films for the presence of cancer or pre-cancerous tumors. (This goes beyond the previous threat of outsourcing film interpretations to low-cost centers in India, for example.)
These medical “expert systems” may ultimately augment or even replace many human healthcare providers making diagnosis today.
However, even the well-publicized entrant into the market, IBM’s highly touted Watson computer, experienced an embarrassing setback when a major Watson implementation at MD Anderson Cancer Centers was deemed a flop — to the tune of a $62 million write-off.
Breakthroughs in Artificial Organ Development and Human Replacement Parts
Finally, we ask: Is the 6 million dollar man walking among us now?
Now that many arm and leg prosthetics have given up the attempt to mimic the appearance of human limbs, they’ve become a cool part human/part android fashion accessory. (So cool in fact, Brazilian Vogue got caught photoshopping fake amputations onto some of its models on a fashion shoot.)
But that’s potentially just the beginning.
Need a liver transplant? How about a liver that’s been grown in a test tube?
As we’ve written before, advanced research at leading edge facilities like the Broad Institute is making astounding progress on developing replacement organs in the laboratory.
While transplanting a lab-grown or 3D printed organ into a human is still ways away from becoming common practice, that’s not the case with 3D printed “bones,” which are now used as graft elements to reconstruct complex structures, such as jaws (whether due to birth defects or injuries). Surprisingly, this technology has been in widespread clinical use for the last 10 years.
https://www.youtube.com/watch?v=yAZ1v0n5_ng
What’s next?
Research in the lab points to true cyborg (part man, part computer) capabilities. Advances in mind control, whereby the human can control prosthetic devices, such as limbs, or eye and ear implants, will become mainstream in the next few years.
Are you ready?
The future is closer than you think.
Turn to Formaspace to Meet Your Future Healthcare Facility Needs

A conversation with your friendly Formaspace Design Consultant can help you plan for the future.
Turn to us for new ideas and concepts to make your laboratory, healthcare facility, or research institute more flexible and efficient.
Find out why leading institutions, such as CVS Health, Cardinal Health, and Florida Hospital trust Formaspace for their healthcare facility needs.
Make the connection today. Fill out the quick form below, and a Formaspace Design Consultant will contact you today.