Fentanyl Abuse is No Longer Just a Prescription Drug Issue, it has become a Recreational Drug Problem with Devastating Consequences
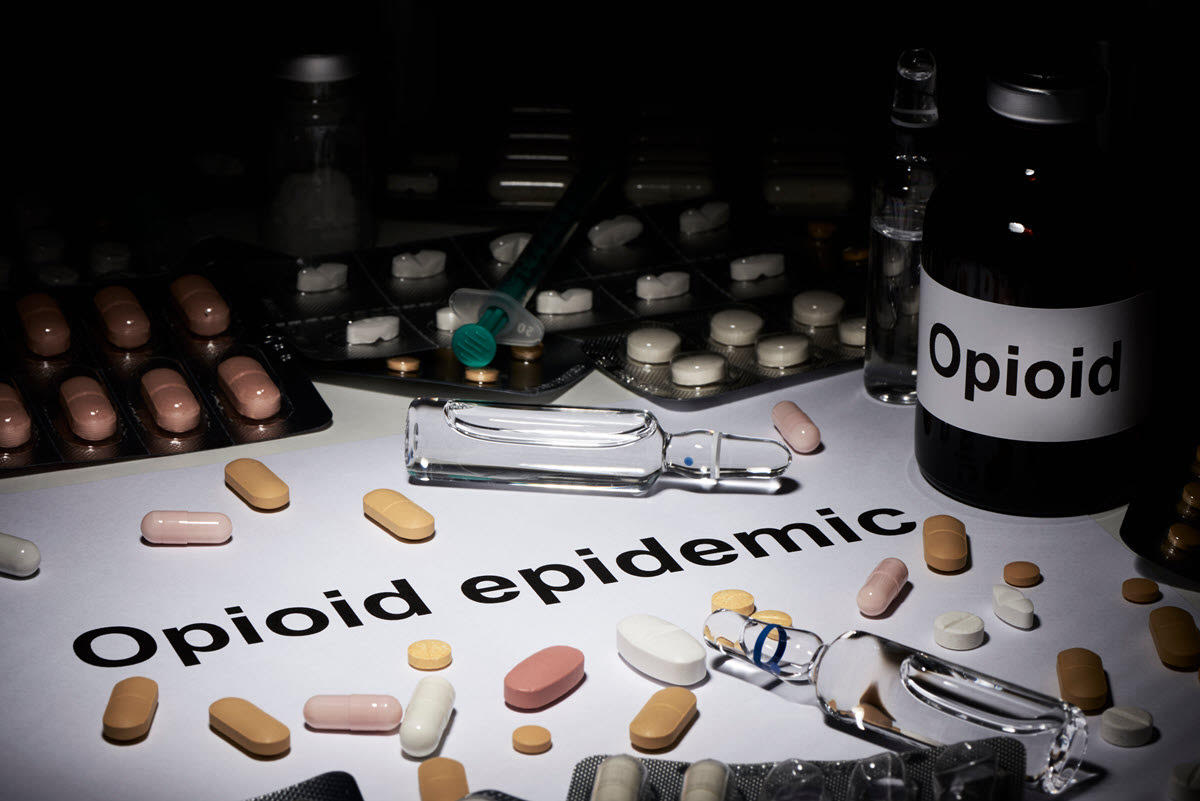
Fentanyl is a powerful synthetic opioid drug that is commonly prescribed for severe pain or used as anesthesia in surgery.
But in recent years, Fentanyl has become infamous as a dangerous, illicit recreational drug, either taken on its own or mixed with other street drugs, including cocaine, heroin, and methamphetamines – oftentimes without the drug user or dealer’s knowledge.
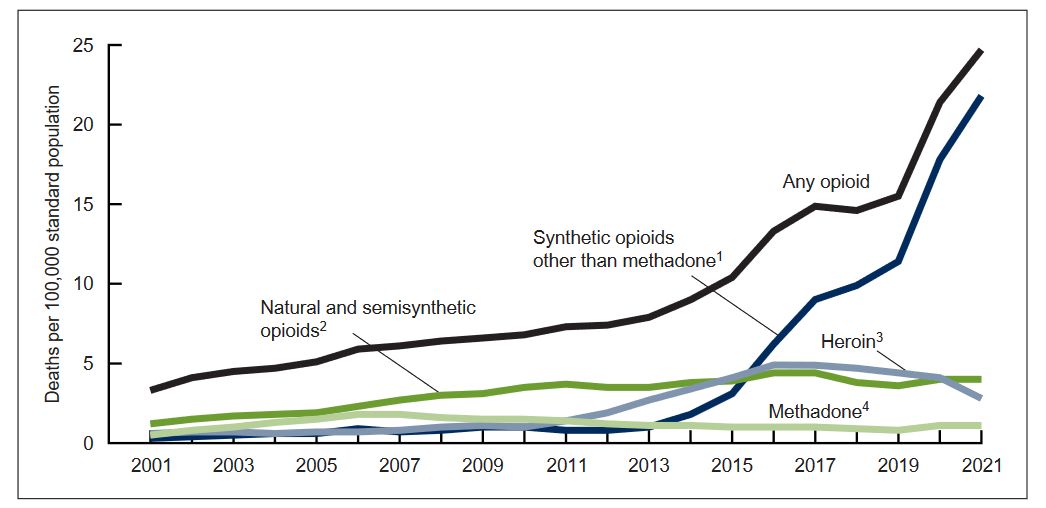
According to the CDC, the number of deaths from overdoses of synthetic opioids (other than methadone) has skyrocketed since 2015, from less than 5 per 100,000 people to more than 20 in 2021.
What is Fentanyl’s Mechanism of Action, and Why is it So Powerful?
What makes Fentanyl so effective as a pain killer, as anesthesia, or as a dangerous recreational drug responsible for so many overdose deaths?
As with other opioids, Fentanyl interrupts the central nervous system’s ability to feel pain.
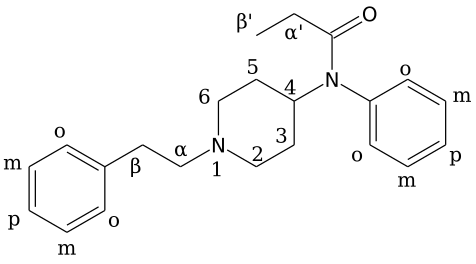
Fentanyl is especially good at this, first of all, because it is very soluble in fats (lipids) – allowing it to move easily throughout the body. Second, it’s 50 to 100 times more effective at binding to μ-receptors compared to Morphine, making it an exceptionally effective pain killer (analgesic) – but one that can also be fatal due to misuse or overdose.
Fentanyl’s pain-killer effects are initiated when it binds to μ-receptors and other G-protein-coupled receptors; this reduces (inhibits) the two-way nervous system communicating pain signals to the brain.
Fentanyl accomplishes this in part by reducing the production of the Cyclic adenosine monophosphate (cAMP) and calcium ion influx while raising the potassium efflux.
cAMP plays an important “secondary messenger” role in communicating signals between cells (including messages from hormones such as glucagon and adrenaline).
So as Fentanyl decreases cAMP production, it disrupts the sending of pain signals to the central sensory nervous system. Without a sufficient number of pain signals to process (nociception), the nervous system won’t mount a protective defense.
In low doses – taken as prescribed under a doctor’s care – opioids such as Fentanyl can be an effective analgesic (pain killer), albeit one with a history of addiction and addiction.
Numbness to sensory pain by itself is generally not fatal. Of course, you could burn yourself on a hot stove more easily due to reduced pain sensation in your fingers.
But the real risk comes from opioid overdose, which can be fatal or lead to permanent brain damage.
People who die from opioid overdose typically succumb to either cerebral hypoxia (a lack of oxygen to the brain) or neurotoxicity (the killing off of neurons in the nervous system).
How does this come about?
As mentioned earlier, Fentanyl binds easily with μ-receptors.
When Fentanyl binds with μ-receptors at high doses, it can lower the body’s rate of breathing (respiratory depression) and reduce the sensation of pain in the brain (supraspinal analgesia).
Fentanyl can also bind with K-receptors, causing sedation (sleepiness) and spinal analgesia (pain-killing effects in the spinal column).
This combination can lead to a dangerous Fentanyl overdose, where the victim first passes out, and if no first aid action is taken, they could die due to a lack of oxygen reaching the brain* (cerebral hypoxia).
(*The human brain typically requires 3.3 ml of oxygen per 100g of brain tissue every minute to function normally.)

Minimizing Fentanyl Exposure Risk to First Responders, Law Enforcement, and the Public
It doesn’t take very much Fentanyl to cause breathing trouble, dizziness, or a possible overdose – as little as 2 milligrams. This is an infinitesimal amount. Imagine a teaspoon of salt grains, that’s about 5000 milligrams. 2 milligrams of salt would be just half a dozen grains.
For this reason, First Responders need to be trained not only to identify the signs of a potential Fentanyl overdose but also the need to protect themselves and those around them from accidental exposure to the drug.
In particular, they need to protect themselves and others from inhalation, ingestion, contact with a mucous membrane, or a needlestick. Avoid eating, drinking, smoking, or using the bathroom when working at a site where Fentanyl is suspected.
First responders should wear appropriate PPE, such as gloves and face masks, and use soap and water to clean their hands rather than alcohol or liquid sanitizers, which could facilitate drug absorption into the skin. Testing of suspected drug samples should be done offsite in a dedicated lab to avoid exposure in the field.
Because Fentanyl users can take the drug in various ways, including by injection, by snorting up the nose, or orally (via pills or by licking blotter paper), anyone coming to the aid of a potential overdose victim needs to avoid touching any drug-associated paraphernalia found nearby, including any white powder, pills, baggies, blotter paper, needles, etc. Fentanyl has also been detected in other illicit drugs, including heroin, cocaine, crack cocaine, and crystal meth, so these items, as well as any other suspicious items nearby, should also be assumed to be contaminated with Fentanyl.
Finally, if the site is a suspected Fentanyl drug lab (or there is drug powder or dust in the air), First Responders should avoid the area and call the nearest DEA field office for the assistance of specialists equipped with full-body PPE and breathing apparatus that are trained in handling hazardous substances.

Signs of a Fentanyl Overdose and the use of Naloxone, an Emergency Opioid Antidote, that Can Help Save Lives
What are the signs of a Fentanyl overdose?
Fentanyl overdose victims will often be found unconscious (for no apparent cause) or show signs of very shallow breathing.
The presence of suspected drugs or nearby paraphernalia (if any) can lead First Responders to assume the cause is related to an opioid overdose.
If the patient can breathe, administering oxygen can help reverse the risk of hypoxia (lack of oxygen to the brain).
If oxygen does not help the patient revive satisfactorily, the anti-opioid drug Naloxone can be administered via injection into a muscle or, if the nasal version is available, via spraying into the nasal cavities. Severe cases may require repeated doses of Naloxone; see the drug information provided by the pharmaceutical company for more information.
How does Naloxone Reverse the Effects of an Opioid Overdose?
Naloxone, available under the brand name Narcan, can reverse the effects of opioid overdoses caused by Fentanyl, heroin, or morphine.
Naloxone is a competitive antagonist that binds to the same receptor protein targets as opioids such as Fentanyl, blocking any remaining opioids in the system from binding. After binding to the receptors, Naloxone reverses the earlier effect of opioid exposure on the central nervous system, stimulating these systems to encourage the patient to begin breathing again naturally, hopefully with enough effect to restore sufficient oxygen to the brain.
Ideally, prompt administration of Naloxone can save a life.
However, because longstanding opioid abusers may experience severe withdrawal systems, Naloxone by itself is not a “one-and-done” long-term cure for addiction. Drug treatment specialists may rely on a series of drug treatments to help wean patients off opioids and other drugs.

The Biden Administration is Encouraging Manufacturers to Offer an Over-the-Counter Version of Naloxone
At present, the anti-opioid drug Naloxone is available via prescription from Emergent BioSolutions, which markets the injectable version under the brand name Narcan, and the naloxone hydrochloride nasal spray version under the name Kloxxado (approved in April 2021.)
Recognizing that anti-opioid treatments could save lives, the Biden administration is encouraging manufacturers to make versions of Naloxone available over the counter without a doctor’s prescription.
Emergent BioSolutions is reportedly considering the request and expects to respond to the FDA by March 2023. Another company, the nonprofit Harm Reduction Therapeutics, has made a fast-track application and hopes to offer Naloxone over-the-counter at cost, including some available at no charge.
That would be helpful according to groups advocating for wider availability of the anti-opioid drug. They point out the high cost of Naloxone has prevented many organizations from stocking the drug as part of standard first-aid kits.
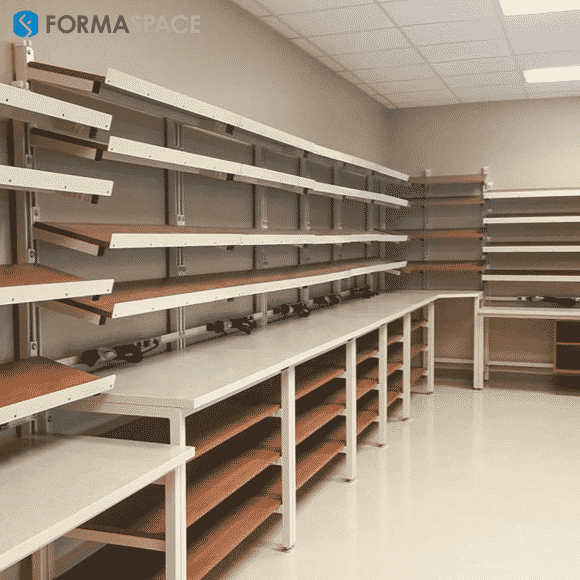
Formaspace is Your Laboratory Research Partner
If you can imagine it, we can build it, here at our factory headquarters in Austin, Texas.
To find out more, contact your Formaspace Design Consultant today.