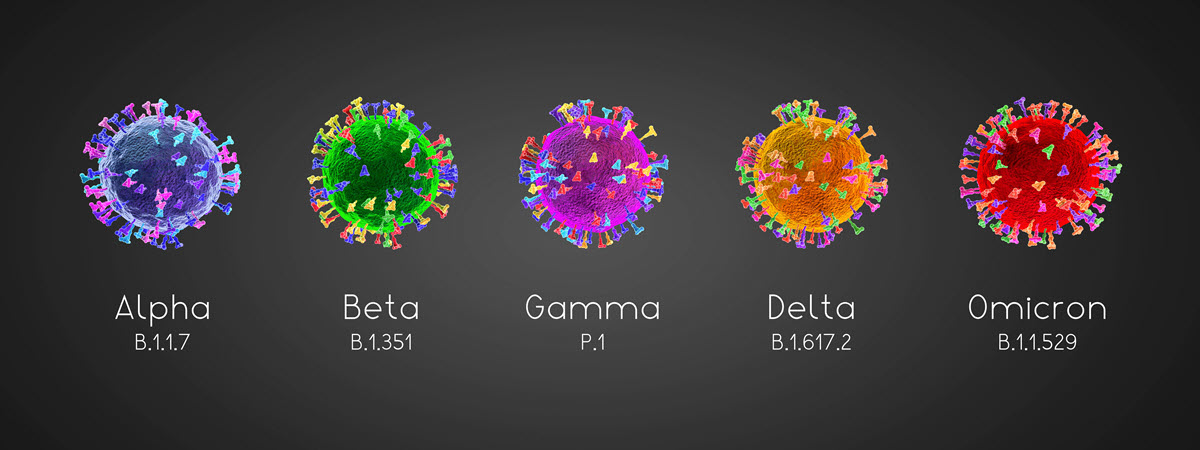
Omicron is the New Unwelcome Guest at the Party
Covid is back in the news – but not in a good way.
The recently discovered new coronavirus variant, dubbed Omicron by the World Health Organization, has now reached the United States with cases identified in 16 states so far. Given its high transmissibility (purported to be much worse than the Delta variant), it’s highly likely Omicron has already spread across the nation. Covid testing and gene sequencing remain a shortcoming in the US public health arsenal (especially compared to other western countries, such as the UK), but ongoing reconnaissance in the invincible sewer treatment plant should soon be able to confirm the spread of the variant across major metropolitan areas.
The problem is we just don’t know yet how the Omicron story will unfold. It will take a few more weeks at least to corroborate early speculation that the disease, while highly transmissible, could produce a milder infection (hopefully so) yet may also lead to more cases of diseases in younger adults and children (a worrying possibility). The genesis of the variance is also under debate, with some researchers speculating that it may have a zoonotic origin, meaning it jumped from humans to another animal species (such as rats) where it acquired multiple genetic changes and then once again spread back to humans. Again, time will tell.
Covid Monoclonal Antibodies and New Antiviral Clinical Treatments May Help Treat Omicron Patients
Since the start of the Covid pandemic in 2020, there has been rapid progress in developing clinical treatments for those who become ill with the virus.
For example, the pharma giant GlaxoSmithKline (GSK), working in partnership with Vir Biotechnology, introduced Xevudy (sotrovimab), a monoclonal antibody drug, which has received Emergency Use Authorization from the FDA to treat patients with active Covid cases. According to a statement from GSK (which has not yet been peer-reviewed), they are confident that Xevudy (sotrovimab) will be effective against the Omicron variant. If true, this may also indicate that Gilead Science’s antiviral Remdesivir and a monoclonal antibody cocktail from Regeneron may also be effective for the clinical treatment of Omicron patients.
Collectively speaking, however, these drugs have a shortcoming in that they require doctor’s care to administer an injection or an intravenous drip – putting additional pressure on medical services that continue to be overwhelmed in some areas of the country where the Delta variant continues to rage.

That’s why antiviral Covid treatments in pill form (which can be prescribed at the pharmacy and administered at home) have attracted so much attention.
The two leading “Covid Pill” candidates, Paxlovid (PF-07321332; ritonavir) from Pfizer and Lagevrio (molnupiravir) developed by Merck (in partnership with Ridgeback Biotherapeutics), have not yet received FDA approval*, but already the Biden administration is hoping to add them the Federal government’s pandemic response plan.
*The Merck drug has been approved for use in the UK and recently received a narrow preliminary FDA committee approval.
Researchers are also investigating the use of other “pill” treatments, such as the anti-depressant Fluvoxamine, which appears to show promise in treating Covid.
Other researchers are also urging the prophylactic use of Vitamin D tablets, as there appears to be a connection with lower levels of Vitamin D and more severe cases of Covid disease among hospitalized patients.
Can We Repeat the Success of Covid Vaccines for the Omicron Variant?
Of course, it’s far better to avoid getting sick in the first place, so much attention is being directed at whether the existing vaccines, particularly the mRNA jabs from Pfizer and Moderna, will offer sufficient protection against the Omicron variant, and, should they fall short, how long would it take to produce new vaccines to ward off Omicron?
The jury is still out on the efficacy of existing vaccines, although Moderna issued a pessimistic statement saying their vaccine was likely to be much less effective against Omicron. Meanwhile, BioNTech, the developer of the Pfizer vaccine, said it might not be until March 2022 until a new version of their vaccine could be put into mass production.
So does this speak to success or failure?
We’d say success. Moderna and Pfizer/BioNTech were able to design and distribute millions of the original Covid vaccines in record time thanks to a combination of several factors:
- Collaboration among scientists, particularly the Chinese researchers who decoded the virus
- Gene decoding technology, which enables us to understand the precise genetic form of the virus in order to create a vaccine that prompts an immune response
- Years of research on how to use mRNA as a delivery mechanism, including how to transport the fragile RNA particles within an infinitesimally small sphere of lipid fat
- Project Warp Speed, the Trump administration’s initiative to put the pharma industry on a war footing and to pay the industry to move to full production even before clinical trials were completed
The results have been astounding.
Unfortunately, highly transmissible variants, such as Delta (and now Omicron) have raised the stakes even higher, with many researchers now believing that achieving herd immunity will require vaccination rates higher than 90%.
Compare that rate to what’s happening in low-income countries, where on average, only a little more than 6% of their populations have received at least one dose of vaccine.
Therein lays the issue. Without worldwide herd immunity, we won’t be able to wipe out Covid, and we may continue to struggle against Omicron, as well as the next variant and the next one after that.
How can Pharma Leverage the new mRNA Delivery Mechanisms?
Let’s shift direction and talk about the impact the development of Covid vaccines and clinical treatments has had on the greater drug development pipeline.

For example, the ingenious mRNA drug delivery mechanism featured in the Pfizer and Moderna vaccines offers a new platform for treating a wide variety of diseases.
· Influenza (Flu)
As we’ve seen with Covid, mRNA-based vaccines can be developed quickly and mass-produced. This could revolutionize the annual flu shot by allowing vaccine developers to create a much more targeted (and thus effective) vaccine against the current year’s expected strain of influenza compared to today’s slower, more imprecise methods.
· Malaria
The newly approved RTS,S malaria vaccine reduces severe malaria by 30%, but an mRNA-based vaccine that addresses malaria’s trick of lulling the immune system’s T-cells into a state of “immune system amnesia” could result in a much more effective vaccine.
· Cancers Caused by Viruses
Cancer is not one but actually a collection of hundreds of diseases – and those caused by viruses, such as the human papillomavirus (a form of herpes) that can cause fatal diseases such as cervical cancer, can be prevented with vaccines. But mRNA-based vaccines offer even more promise in targeting one or more gene mutations, helping to extend the life of cancer patients or, in some cases, even eliminating the mutated cells entirely for full remission.
Drug Development Pipeline Remains a Bottleneck
We should have included another “success factor” in our list of reasons why the Covid vaccines were developed so quickly: the Covid virus (aka SARS-CoV-2) has a relatively obvious and straightforward target, the spike protein that gives it its name Coronavirus – from the Latin word corona, or crown. Teach the human immune system to recognize the spike (by temporarily flooding the body with “spike-alikes”), and you can get a good immune response.
But not all diseases are so straightforward. Take HIV, for example. Research has been ongoing since the disease first was identified in the 1980s, and although we now have excellent drugs to control it (or prevent it, via PREP, for example), its tricky pathology has thus far evaded a simple cure.
Once an effective treatment for HIV is found, it very well could be a candidate for delivering the API (active pharmaceutical ingredient) directly into the cells via an mRNA-based vaccine or clinical therapeutic.
This brings us to the ongoing challenge of effective drug discovery and development.
We’re getting better at delivering drugs, but it’s still as difficult as ever to develop new active ingredients for complex diseases, such as HIV.
Evidence Still Points to Smaller Pharma Companies Having the Edge in Drug Discovery
No one wants to solve this long-standing drug development pipeline problem more than the large pharma companies.
They would love nothing more than to achieve a predictable (and profitable) product introduction calendar and thus avoid relying on the boom-and-bust cycle of blockbuster drugs, whose introductory profits skyrocket to new highs only to crash earthward years later when the drug patents run out.
Frustratingly for the pharma giants, the smaller companies still seem to have the edge in innovation – you only have to witness the peppering of smaller company partnerships mentioned in this article so far, including BioNTech, Ridgeback Biotherapeutics, and Vir Biotechnology, to see that there is an issue from the larger pharma company point of view.

Will AI Unleash a Golden Era in New Drug Development?
One long-standing solution to this problem is for pharma giants to acquire smaller companies with innovative products in the drug development pipeline. But this approach is expensive – especially considering that many pharma giants are already paying for their own large lab facilities and research scientists.
But there is a new savior on the horizon.
Big pharma companies are eyeing the potential of AI to power their drug development pipelines.
Indeed there is so much investment and activity in pharma-based AI research now that this new trend would undoubtedly be the industry’s top headline story for both 2020 and 2021 had not the Covid pandemic come along to steal the spotlight.
Record investments in pharma-focused AI startup companies during 2020 and 2021 underscore the point.
Here is just one example: the AI drug discovery startup Valo recently raised $2.8 billion in a SPAC merger.
Key AI initiatives and Partnerships in the Pharma Industry
But the bigger story is how tech giants are starting to enter the AI-based pharma market and the corresponding rush by major pharma companies to establish their own joint AI partnerships, including:
· Alphabet (Parent of Google)
Leveraging its massive bank account and the success of its Deep Mind AI engine (which has resolved complex protein folding problems once thought to be impossible), Google’s parent company Alphabet is poised to use its AI expertise to jump into the drug discovery market.
· AION Labs: Joint Venture between AstraZeneca, Merck, Pfizer, and Teva
AstraZeneca, Merck, Pfizer, and Teva are joining forces with Amazon Web Services (AWS) and the Israel Biotech Fund (IBF) to create a new AI-consortium dubbed AION Labs that will leverage AI and cloud-based computing technologies to speed up the development of new therapies.
· Nvidia Partnership with AstraZeneca, Schrödinger, University of Florida
Austin-based AI and graphics chip computing powerhouse Nvidia has announced a partnership with AstraZeneca, Schrödinger, and the University of Florida to leverage Nvidia’s transformer-based neural network architecture MegaMolBART to facilitate rapid reaction prediction, perform molecular optimization, and create new designer molecules.
· Sanofi and SRI
French pharma giant Sanofi has announced an AI-focused drug discovery collaboration with the famed Silicon Valley-based think tank SRI (formerly Stanford Research Institute). SRI is developing DASLTM (Deep Adaptive Semantic Logic) – an AI-based molecular design tool for multi-parametric optimization.
· Facebook Alum Tom Stocky and Insitro
Facebook developer turned biotech exec Tom Stocky was recently named president of the San Francisco-based startup, Insitro, a machine-learning drug discovery and development company.
What are the Potential Ways AI can Accelerate the Drug Development Pipeline?
How can AI be used to accelerate the drug development pipeline? Here are five key ways pharma companies plan to focus their AI research:
· Analyze the Massive Data Collected by Electronic Medical Records and Next Generation Sensors
In the last ten years, Electronic Medical Records have become ubiquitous, spurred in part due to the provisions in the Affordable Care Act, better known as Obamacare. Leading EMR vendor Epic alone has accumulated over 122 million patient records in its Cosmos database, just one example of the rich source of big data that can be mined by sophisticated AI tools to identify better clinical outcomes to support new evidence-based medicine protocols. In addition to medical records, new smart medical sensors are another up-and-coming technology that will add to the ever-increasing collection of patient data, ready to be analyzed by AI-powered big data tools.

· Identify Promising Drug Compound Candidates
Pharma companies also hope to harness the power of AI to bring order to the process of evaluating drug compound candidates, a process that here-to-fore has been one of either based on informed scientific “hunches” (as was the case with the development of Remdesivir now being used to treat Covid patients) or a slow, deliberate process more akin to gruntwork – where every potential drug compound is laboriously tested against different diseases. It’s hoped that AI-based big data tools can speed up this process by months (if not years) by matching molecular profiles with the need to encourage or inhibit biological processes responsible for disease.
· Design New Drug Compounds from Scratch
If AI-powered big data tools can successfully identify potentially useful drug candidates from existing compounds, why not go a step further and create “designer drug” compounds from scratch? This idea has now taken hold among researchers. One approach is to first model the biological process of the human body, to create in effect a “digital twin” that can represent both healthy and diseased biological models – serving as a jumping-off point for designing compounds to either inhibit or assist biological processes that cause/cure disease.
· Optimize AI-Powered Gene Splicing (CRISPR)
Refining drug candidate molecules into practical active pharmaceutical ingredients (APIs) often requires editing extracted key bits of genetic code from longer molecular chains or breaking molecules apart so they can be analyzed or replicated for further study or processed for use in a drug compound. There is also interest in using the CRISPR gene-splicing technology in combination with AI-based research tools. UC Berkeley professor Patricia Doudna, who we have written about before, is leading a new venture called Mammoth Biosciences, whose goal is to create medicines that perform gene editing directly in the body. Meanwhile, gene editing startup Caribou raised an initial $304 million in its effort to fund development of its non-Hodgkin lymphoma therapy.
· Organize Human Drug Testing Trials and Analyze Results
As we have seen with Project Warpspeed’s Covid vaccine development, successfully organizing and interpreting human drug testing trials to the satisfaction of the FDA is a major bottleneck in the drug development process. Pharma companies are investing in AI-based tools with the expectation it could help significantly reduce both the time and costs associated with clinical trials while increasing the understanding of a drug candidate’s efficacy.
Can AI Technology Help Address other Pressing Needs in Clinical Therapy?
The five areas detailed above, if successful, would validate the large investments pharma companies are now pouring into AI-based drug development.
But could AI do more?
Here is our Christmas wish list for three more achievements that AI-based medicine might help bring about:
· Avoid Bias in Drug Development and Medical Device Testing
AI in general has been accused of amplifying unintentional bias, so this is an opportunity to show that AI-based tools can do the opposite, e.g. undo years of bias in drug development and medical device testing. For example, women and minorities are often underrepresented in drug trials, which has sometimes led to inappropriate dosages, mischaracterization of side effects, and more. Medical devices are not immune from this either; medical ethicists have recently pointed out that even simple devices, such as fingertip oximeters that are inaccurate for those with darker skin, leading to inappropriate clinical treatment in Covid cases, for example.
· Improve Orphan Drugs Economics and Speed of Delivery
One area in mainstream drug development that is often left behind is the so-called “orphan drugs” for less common diseases. Without a big potential market, many pharma companies choose to focus their resources on more common diseases that would offer a larger financial payout, leaving the US (via the Orphan Drug Act or ODA) or EU government to find these efforts and smaller non-profit organizations to lead the charge. It’s hoped that AI-based drug development tools could reduce the cost (and time needed) to develop orphan drugs, allowing for more patients to receive life-giving clinical treatments.
· Stay Ahead of the Looming Crisis in Anti-Bacterial and Anti-Fungal Drug Resistance
During the Covid lockdown, the public became quite aware of the need for increased sanitation and hand-washing to prevent spreading the virus. However, multi-drug resistant bacteria and fungal infections, collectively known as Super Bugs, continue to be a looming major threat that could upend nearly a century of progress brought about by antibiotics (penicillin was first discovered in 1928.) Hopefully, AI-based drug discovery tools will help identify or design capable new weapons in this war against Super Bugs.
Some Final Thoughts on the World of Clinical Medicine beyond AI
Drug development does not happen in a vacuum. In addition to scientific research in the lab, we need to zero in on identifying and achieving better outcomes in public health policy.
· Emergence of New Covid Variants Underscores the Need to Make Public Health a Global Priority
The emergence of new Covid variants is a tragedy; one that may yet be repeated again even after the Omicron variant has taken hold across the world. It’s in our own selfish interest to see off diseases such as Covid – and other so-called “third world” diseases (which could easily spread here in future if we are not careful) by investing in public health campaigns around the world, such as vaccinating poorer countries against Covid. Similarly, we applaud international agreements, such as the recent proposal for a global pandemic treaty moving through the United Nations, that could help hasten a faster, more effective, and comprehensive response to the inevitable “next pandemic.”
· Don’t Overlook the Need to Focus on Educating the “Public” in Public Health
Misinformation about vaccination has become a big business. It’s time for public health to take back control. One place to start is by cleaning house in the drug approval process at the FDA, which needs to be more transparent and avoid the type of controversies surrounding the approval of the Alzheimer’s drug Aducanumab. And the public needs more information on how the drug approval process works too, in order to increase trust in the system. For example, a recent poll found that only 10% of US adults were aware that it normally takes between 10 and 15 years to bring a new drug to market.
· The New Drug Development Revolution Will Need a Deep Bench of Trained STEM Workers
If the AI-based drug development revolution is to be successful, we will need a lot more highly-trained STEM workers to fill the positions in biotech and computer science. We need to ramp up the education of these workers now, as they are already in short supply, with companies falling all over each other to attract the best talent.
· Public Health is a Global Issue. But Pharma Manufacturing Needs to Go Local for National Security
Finally, the Covid pandemic taught nations around the world that security begins at home, with local production of pharmaceuticals and PPE. We need to promote policies that encourage reshoring of PPE and pharma product development and manufacturing capabilities here in the USA, just as other countries need to expand their own domestic production capabilities.

Formaspace is Your Pharma Laboratory and Manufacturing Partner
If you can imagine it, we can build it, here at our factory headquarters in Austin, Texas.
Formaspace manufactures custom laboratory solutions (from single workbenches to full lab installations) as well as building one-of-a-kind industrial furniture to make your manufacturing, fill and finish operations and packing and shipping facilities operate with greater efficiency.
Talk to your Formaspace Design Consultant today and find out why pharma companies choose Formaspace for their laboratories and manufacturing ops.