In this article, we take a look at the many important recent developments in cancer research.
But first, we should address the effect of the Covid pandemic on cancer research and the Life Sciences sector in general.

As you might expect, Covid has been a disruptive force over the past year, with many cancer research personnel having to adjust to working from home and many labs requiring updates to their facilities, including improving their ventilation systems, installing transparent barriers between lab stations, etc.
Cancer clinicians have also bemoaned the fact that during the height of the pandemic, many patients avoided coming into healthcare facilities at all – a troubling development for those who could have benefited from early cancer detection screening – when clinical treatment is easiest, and outcomes are most promising.
As a result, it’s widely believed we’ll see a significant uptick in cancer detection in the coming months as people return to healthcare facilities for regular screenings.
Many ongoing cancer drug trials were also disrupted by the pandemic as patients hesitated to sign up or elected to withdraw out of concerns over the Covid virus.
On the other hand, there have been some rare positive developments in the Healthcare and Life Sciences industry due to the Covid pandemic:
- One notable development is that the US did not experience any widespread influenza outbreak during the past “flu season,” presumably due to increased personal hygiene, including frequent handwashing as well as widespread mask wearing during the pandemic.
- Thanks to the rapid development and early success of Covid vaccines, there is renewed interest in life science research (including disease research and prevention) by the public, government officials, tech companies, investors, and the media.(We’ll investigate the current rapid growth of the Life Sciences sector in an upcoming series of articles.)
- The FDA and other drug regulators around the world have given provisional (emergency use) approval for RNA-based vaccines from BioNTech and Moderna, validating an approach championed by the once overlooked researcher Kati Kariko. This approval of RNA-based vaccines could greatly speed up the acceptance of other RNA-based therapies that pharma companies have in development, including so-called “cancer vaccines,” which we investigate below.
Could the Success of Covid Vaccines Point the Way to New Funding Models for Disease Research?
There’s a fourth point as well.
The widely viewed success of “Operation Warp Speed” – the government initiative to provide massive funding to private companies seeking to develop a workable Covid vaccine as fast as possible (while shielding them from potential product liability) – has demonstrated that increased government funding support (and effective management) can deliver results.
This has increased calls to reassess (and hopefully increase) the role of public funding in drug research, with some scientists pointing to the groundbreaking research of Andrew W. Lo and Roger M. Stein, who, along with financial expert John Hull, wrote the 2019 paper “Funding Long Shots” that calls for a completely new funding framework (including Wall Street backing) to provide investor-backed financial support for disease research, including the search for new cures for cancer.
In a world of what many consider highly speculative investments (including SPACs, NFTs, DogeCoins, and the like), one has to believe that increased investment in health research would be a better bet in creating long-term positive change for our society than the alternatives.
The Biden administration has also taken notice of the calls for increased government support and has beefed up funding requests for Life Sciences (including cancer research) in the Recovery Act that passed earlier this year, as well as the proposed Federal Budget and Infrastructure bill.

Hopefully, this new funding will find its way to the likes of the NCI Experimental Therapeutics (NExT) program, which is the National Cancer Institute’s own “mini Operation Warpspeed” that helps coordinate funding for the most promising or novel cancer therapies – from the earliest stages of research all the way through to human clinical trials.
Which are the Most Common Cancers Today?
Let’s turn our attention now to the latest research in cancer diagnostics, starting with the newest cancer incidence rankings.
At 11.7% of all cancers, breast cancer is now the number one most commonly diagnosed cancer world-wide, having supplanted the incidence of lung cancer (11.4%) – a drop that’s possibly linked to long-running anti-smoking campaigns. The next most common cancer diagnoses on a worldwide basis are colorectal (10%), prostate (7.3%), and stomach cancer (5.6%). In the US, the 2020 rankings are similar, except prostate cancer diagnoses outnumber those of colorectal cancer.
What about long-term trends?
Thanks to improving outcomes for breast and prostate cancer, researchers predict the most deadly cancers in the year 2040 will be lung cancer (with the highest level of mortality), followed by pancreatic cancer, liver and intrahepatic bile duct cancer, and colorectal cancer.
There is also concern about the rise in cases of esophageal cancer (esophageal adenocarcinoma or EAC), particularly among adults under age 50. (Cases have reportedly risen nearly 3% per year between 1975 and 2015.) Early detection is key to better outcomes, so those with acid reflux or other sources of discomfort when swallowing should be screened for EAC right away.
Widespread Acceptance of New Cancer Diagnostic Methods, such a Genomics
One of the most important developments in cancer diagnosis is the widespread acceptance, by the medical community and patients alike, of genomics (e.g. DNA testing) as a basis for creating unique treatment plans, known as either Precision Medicine (e.g. therapies designed for a group of individuals that share a common DNA signature, such as triple-negative breast cancer), or Personalized Medicine (e.g. therapies created for individual patients based on their unique set of genetic markers).

Intensive medical data collection and statistical number-crunching are also helping cancer researchers identify which therapies produce the best outcomes (an approach known as evidence-based medicine).
In what can be called a virtuous circle, new cancer diagnostic technologies are being added to this research arsenal all the time.
One of the newest ideas is a Liquid Biopsy approach to evaluating breast cancer risk. It uses extracted fluid to detect levels of cell-free DNA (cfDNA) and circulating tumor DNA (ctDNA), which can help predict breast cancer disease recurrence and adverse survival results as well as predict the potential for metastasis of the axillary lymph node.
Liquid samples can also be used to detect signs of prostate cancer in men using a convenient urine test that can be administered at home.
Innovations in Treating Cancer with Immunotherapy
One of the biggest changes in cancer treatment has been the focus on using the body’s own immune system to fight cancer – an approach known as Immunotherapy – which can help reduce or, in some cases, eliminate the need for more invasive approaches, such as surgery, radiation, or chemotherapy.
There is often confusion between the terms Immunotherapy and Targeted Therapy. Broadly speaking, Immunotherapy treatments encourage the body to rise up and fight cancer (or other illnesses) by boosting the tools of the body’s own immune system. Targeted Therapy, as we’ll see below, goes beyond the capabilities of the body’s existing immunize system to disrupt, disable, and kill cancer cells or tumors by attacking one or more of the cancer’s specific weaknesses as a parasitic intruder in the body.
· CAR T-cell Therapy
CAR T-Cell Therapy is an important new type of gene therapy that is helping patients with cancers that circulate in the blood, such as leukemia and lymphoma.
The therapy involves extracting and separating patient’s T-cells from their blood supply. The T-Cells are then synthetically upgraded using a genetic engineering process to add a new receptor on the T-Cell surface, called a chimeric antigen receptor, or CAR, that’s designed to recognize a specific cancer cell antigen – and kill it.
These modified T-Cells are then mass-produced in the laboratory before they are injected into the body, often after the patient has had other treatments (such as chemotherapy) to reduce the overall number of cancer cells remaining.
It’s critical that the antigen that’s selected does not present on normal, non-cancerous human cells, or the patient could suffer from harmful cell loss or even death.
· Monoclonal Antibodies
Cancer researchers have also discovered that they can boost the existing antibodies found in the body’s natural immune system.
Scientists have discovered that some types of cancer, such as metastatic triple-negative breast cancer, have antigens that are easily recognized by antibodies.
As with T-Cells, the antibodies can be extracted from the body and then massively duplicated in the laboratory to create a large army of monoclonal antibodies (mAbs or Moabs), which can then be reinjected in the body where they can attack the malignant cells.
· Immune Checkpoint Inhibitors
One of the common failings of the immune system when dealing with cancer is distinguishing between normal cells and cancerous ones.
Very often, cancerous cells can “hide in plain sight” by passing themselves off as normal cells. Immune checkpoint proteins probe the surface of different cells – if they can bind to it, then they think everything is OK and send out an “all clear” signal telling the T-Cells to move along and not attack the cell.
The idea behind Immune Checkpoint Inhibitors is to add a bit of protein to the surface of cancerous cells to prevent (e.g. inhibit) the immune system from sending out an all-clear signal in the first place. As a result, the T-Cell will kill off the cancerous cell.
This approach is very effective at first, but, unfortunately, it wears off eventually in many cases, so researchers are looking at ways to improve its long-term efficacy.
· Oncolytic Virus (OV) Therapy
The use of Oncolytic Virus (OV) immunotherapy can be described as setting off a fire alarm in the body, which calls the immune system’s “fire brigade” to spring into action. So far, the FDA has only approved this therapy for inoperable melanoma, using a genetically modified herpes virus that trigger’s the body’s natural immune response to the presence of dangerous skin cancer.
· Cancer Vaccines
Another exciting area in cancer immunotherapy is the introduction of cancer vaccines, such as the first FDA-approved prostate cancer vaccine, sipuleucel-T, which is sold under the brand name Provenge.
We can expect a lot of new developments in this area now that the RNA-based Coronavirus vaccines from Pfizer/BioNTech and Moderna have been provisionally approved by the FDA.
In fact, prior to the Coronavirus outbreak, both BionNTech and Moderna were investigating using RNA-based technology to treat a variety of diseases. BioNTech, in particular, was developing a series of RNA-based cancer vaccines that took personalized medicine to new heights by producing individual cancer vaccines in the lab that were customized for each individual patient.
Researchers are also trying to understand the role that epigenetic changes play in causing cancer. Epigenetic changes are small, taking place at the so-called micro-RNA level, and scientists are looking at micro-RNA therapies to control cancer tumor growth.
Finally, ongoing advances in Crispr gene editing technology are also expected to help further efforts to create new cancer vaccines and other immunotherapies.
(We first wrote about Crispr technology in 2015. In 2020, Emmanuelle Charpentier and Jennifer A. Doudna were awarded the Nobel Prize in Chemistry for their research in developing Crispr gene editing technology, the first time two women have won this prestigious award.)
· Microbiome-Based Therapy
We mentioned earlier the importance of a well-balanced diet in preventing cancer. Good eating habits help maintain a balanced, protective microbiome in our digestive system that can help protect us from cancer. When the flora in our gut gets out of balance, we can get into trouble. For example, scientists are researching the connection between colorectal cancer and the presence of Fusobacterium bacteria and whether antibiotics controlling the bacteria could help reduce this type of cancer.

· Nanoparticle-Based Therapy
Scientists are also exploring the potential of fighting cancer on an even smaller playing field by employing nanoparticle-based therapies. In one recent study, researchers developed a nanoparticle that trains immune cells to attack melanoma cancer in mice.
New Targeted Therapy Approaches to Cancer Treatment
In contrast to immunotherapy, which relies on using the body’s own immune system to fight cancer, targeted therapy seeks to disrupt (and destroy) cancer cells and tumors by attacking weaknesses in the cancer cells themselves.
To achieve this, we first have to identify what characterizes malignant (cancerous) cells from “normal” ones and then come up with potential strategies to subvert or counteract the cancerous cells.
According to a paper published in Cell by Douglas Hanahan and Robert A Weinberg, there are six ways useful ways (in a therapeutic sense) that the behaviors of cancer cells are differentiated from that of normal cells:
- Self-sufficiency in growth signals (oncogene addiction)
- Insensitivity to growth-inhibitory signals (loss of tumor suppressors)
- Evading programmed cell death (anti-apoptosis)
- Limitless replication potential (aberrant cell cycle)
- Sustained angiogenesis
- Invasion/metastasis
See an online graphic of this chart from the authors in JPG or PPT format. Reference: Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000 Jan 7. 100(1):57-70. [Medline].
In layman terms, we can translate the list above (sometimes called “the Hallmarks of Cancer”) into easy to understand terminology:
- Cancer cells receive continuous signals to keep growing
- Cancer cells don’t respond to stop signals telling them to stop growing
- Cancer cells don’t respond to signals to die off (like regular cells do)
- Cancer cells reproduce without limit
- Cancer cells can create new blood vessels in the body to support tumors, for example
- Cancer cells can establish new growth areas in other areas of the body
The challenge for cancer researchers is to create a targeted therapy that interrupts one or more of these characteristics, which in turn reduces the incidence of cancer or even eliminates it entirely.
Two drug categories have emerged in recent years to do this.
· Kinase Inhibitor
The first class of drugs are the Kinase Inhibitors, which block kinase enzymes that are used to sent messages to cells in the body. Since some cancer cells may be more reliant on kinase enzymes to control metabolism and division than regular cells, blocking these communication pathways can help prevent cancer cells from growing.
· PARP Inhibitors
The second class of targeted therapies that have shown promise in recent years are PARP Inhibitors. PARP (short for poly adenosine diphosphate-ribose polymerase) is used by cells to repair damaged DNA. In certain types of cancers, PARP inhibitors (e.g. designer drugs that reduce the ability of PARP to function, e.g. repair DNA) have a greater effect against malignant cells than normal cells, causing them to die off faster than regular cells, thus shrinking tumors in some cases.
Promising New Combination Therapies for Cancer Patients
The long-term side effects of traditional cancer treatment can be significant. For example, many female cancer survivors who received high doses of radiation as part of treatment for breast cancer are being diagnosed decades later with heart valve or other heart damage that may be traced back to radiation therapy.
That’s one reason that cancer researchers are evaluating combinations of therapies, both new and old, to find the most promising courses of treatment that also minimize the potential harmful short-term (and long-term) side effects.
This can be good news for some of today’s cancer patients, who might be able to be successfully treated with a combination of immunotherapy and targeted therapies.
Even if these new, innovative courses of treatment are not sufficient to cure their cancer, these new treatment regimens can often reduce the need for follow-up surgery, radiation, or chemotherapy – or reduce the number of radiation treatments or rounds of chemotherapy required, which is a significant benefit for the patient.
More research is needed, and we believe added financial support from Washington will help further the cause of finding new clinical therapies to treat cancer.

New Insights into Cancer Prevention
Fortunately for most of us, our genes are not 100% determinative of our destiny when it comes to cancer diagnoses.
Researchers keep finding that each of us can exert significant control over our health – and help prevent the onset of cancer – by perusing healthy lifestyle choices, such as exercising regularly and eating a healthy diet (to create a healthy, cancer-fighting microbiome in our digestive system).
Quitting smoking remains the most important step we can take to prevent lung cancer – and possibly (according to new research) breast and prostate cancer.
Even second-hand smoke is more dangerous than we thought. A new study finds that second-hand smoke can raise the risk of oral cancer by as much as 51%.
Maintaining a healthy weight can also help prevent the onset of cancer. Obesity is now considered (after smoking) the second-leading cause of preventable cancer deaths in the US.
A recent study on the benefits of Vitamin D suggests that not only could Vitamin D deficiencies aggravate the seriousness of Covid-19 illnesses, Vitamin D supplements could help prevent cancer deaths, especially for those over 50.
Researchers are also investing in the intriguing possible connection between night-time light pollution, known as Lighting at Night (LAN), and the incidence of thyroid cancer. The presentence of artificial light during our sleep is thought to interrupt the body’s circadian rhythm, including production of melatonin and other hormones, such as estrogen.
When you go to bed at night, it’s time to turn off electronic devices and hang blackout curtains over the windows to get a better night’s sleep!
Formaspace Is Your Life Sciences Lab and Manufacturing Partner
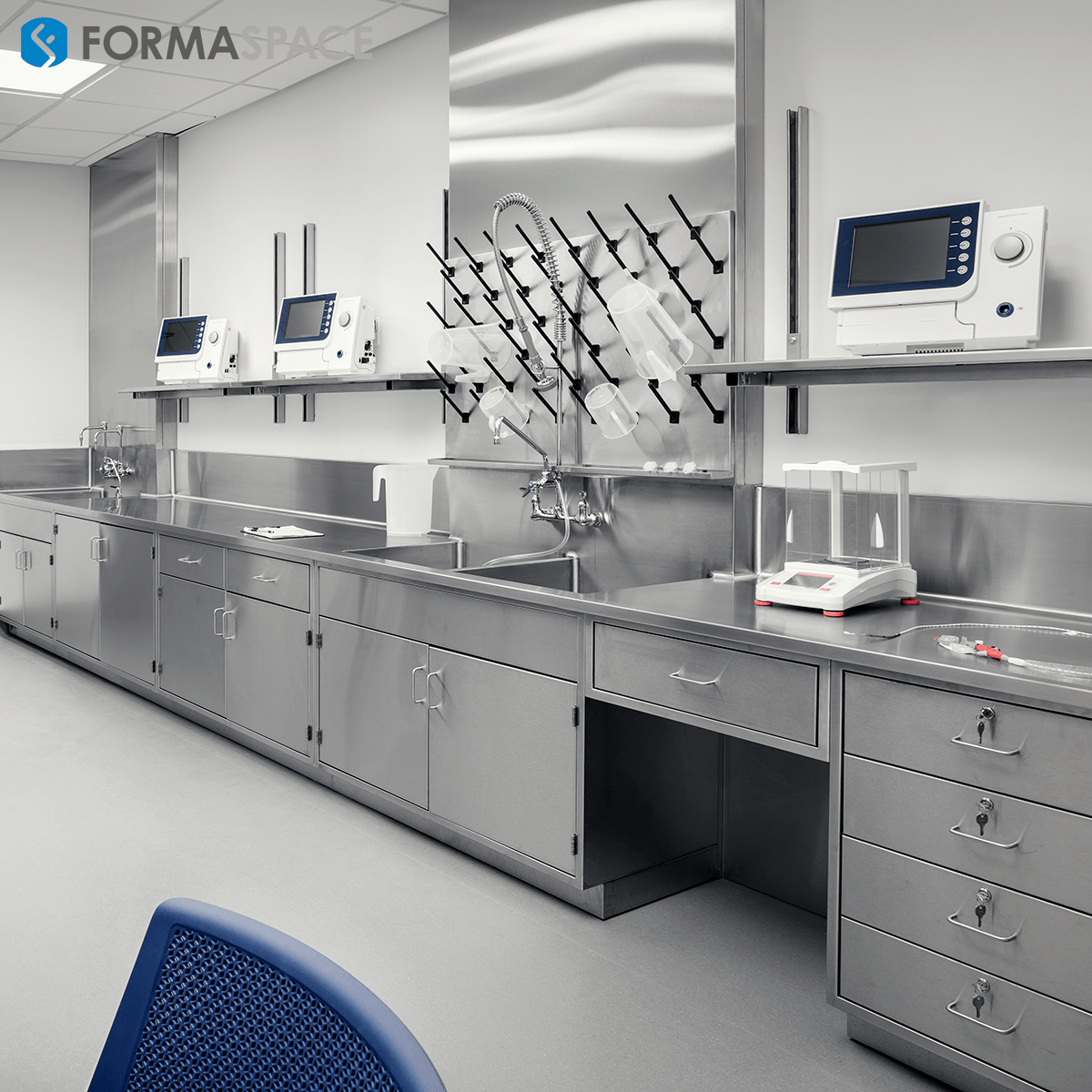
If you can imagine it, we can build it – here at our factory headquarters in Austin, Texas.
The life science specialists here at Formaspace can work with you to develop custom furniture solutions to improve the efficiency of your life science center, healthcare research laboratory, clinical testing lab, pharma manufacturing facility, or educational facility.
Now is the time to find out more.
Contact your Formaspace Design Consultant today and find out why leading names in the pharma and biotech research and manufacturing industry, including Roche and Chan Zuckerberg Biohub, choose Formaspace.